Parkinson’s disease
Parkinson’s disease is a progressive neurodegenerative disease that primarily affects the parts of the brain that control movement, resulting in tremors, stiffness, and slowness. Some people living with Parkinson's may also develop dementia in the later stages of the disease.

Overview
Parkinson’s disease (often shortened to PD) is a progressive neurodegenerative disease that primarily affects the parts of the brain that control movement. This results in tremors, stiffness, and slowness, while difficulty walking and loss of balance typically emerge as the disease progresses.
Some people may also develop dementia as their PD progresses into the later stages of the disease, often resulting in significant memory loss and difficulty concentrating, thinking, completing routine activities, and navigating the environment. Behavioural problems are also common including depression, hallucinations and delusions.
Idiopathic Parkinson’s disease is another name used for PD.
Symptoms
The age of symptom onset and the progression of PD can vary among people; however, as PD is a progressive degenerative disease, symptoms will gradually worsen with time.
Symptoms of PD are most commonly seen in people over the age of 50 but may begin under the age of 40.
Difficulties with movement
Early symptoms of this disease are often related to difficulties with a person’s movement. These difficulties with movement may be experienced in one or both sides of the body. People with PD may experience movement difficulties, including:
- Rigidity
- Tremors
- Bradykinesia (slowed movements)
- Loss of balance, or
- Falls.
People with PD may also complain that they feel “stuck in place” when they try to start walking.
Changes in mood and personality
In addition to movement symptoms, a person with PD may experience changes in their personality, such as irritability, depression and anxiety.
Physical symptoms
Sleep disorders, changes in appetite, dry skin, low blood pressure upon standing and excessive sweating are among the physical symptoms of PD.
Dementia-related symptoms
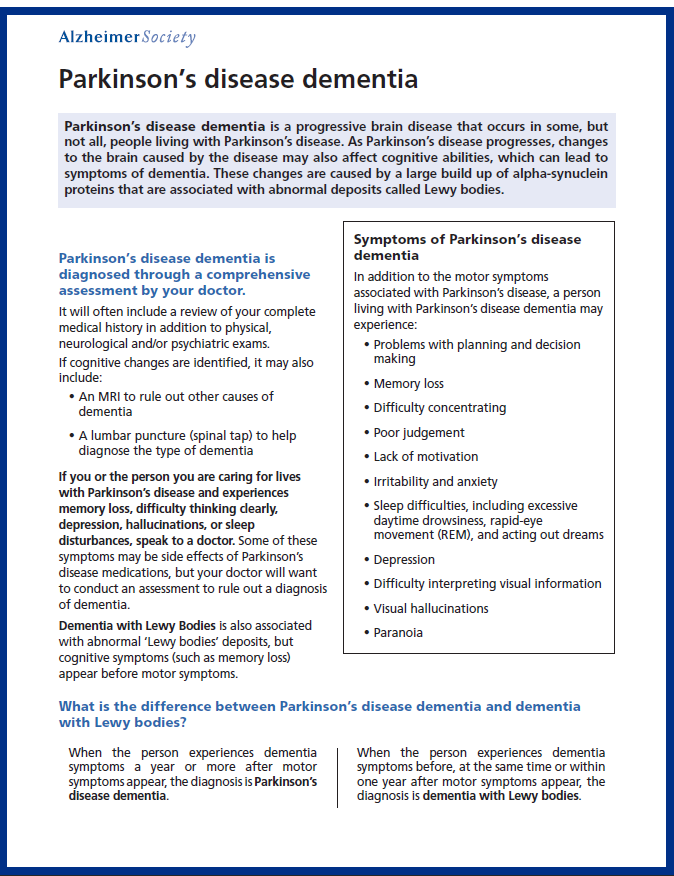
With the progression of PD, some people will experience changes in their cognitive abilities and may develop dementia. People with cognitive symptoms of PD typically experience difficulties with memory, concentration, carrying out routine activities, and thinking quickly.
Visual hallucinations and the inability to control emotions are also common features of the dementia associated with PD. These symptoms have a tendency to fluctuate, causing them to seem better or worse at different times.
Diagnosis
It can be challenging to diagnose PD as there is no single test to identify it, and there are a number of symptoms that are shared with other medical conditions.
The amount of time that it takes to get a PD diagnosis can vary as it depends on a number of different factors, such as:
- Age,
- Medical history, and
- The symptoms present at the time.
Medical history and exams
To help make a PD diagnosis, your doctor will often conduct a comprehensive assessment that may include physical, neurological and psychiatric exams, together with a review of your complete medical history (including a review of current and past medications that could be causing some of the physical symptoms). This thorough assessment helps your doctor rule out other conditions that could be causing the symptoms.
Diagnosis is generally made and confirmed by a neurologist. Diagnosis is typically based on a common pattern of symptoms including tremor, rigidity, and slowness as well as through a detailed physical examination confirming the typical features of the disease.
People living with PD are at an increased risk for developing dementia. Should you be diagnosed with PD, make regular appointments with your doctor so they can monitor you closely for changes in your cognitive abilities.
Brain imaging
If cognitive changes are identified, a physician may request a magnetic resonance imaging (MRI) test to help detect any structural changes in the brain that could be causing the changes in cognition.
Risk factors
At present, there is no known cause of the majority of cases of PD. However, rare genetic abnormalities can sometimes be inherited in families that cause the disease.
Some risk factors have been identified as playing a role in the development of PD, including:
- Age – the risk of PD increases with age,
- Gender and sex – men are at an increased risk of PD, and
- Genetics – having a close relative with PD increases the risk of developing the disease.
Similar to other neurodegenerative disorders, like dementia with Lewy bodies, PD is characterized by an abnormal clumping of a natural protein – called alpha-synuclein – in brain cells.
These abnormal deposits are called “Lewy bodies,” after the scientist who first described them. It is still unknown what causes the formation of Lewy bodies, and why they result in the deterioration of brain cells but researchers believe that these deposits could be linked to the cause of PD.
Treatment
Currently there is no known cure for PD, although people can live with the disease for many years.
Medications
Medications are often used to manage the symptoms of PD. Medications such as Levodopa can lessen people’s challenges with movement.
Medications used in Alzheimer’s disease—such as cholinesterase inhibitors—help to increase brain acetylcholine levels and can also be used to improve symptoms of dementia associated with PD.
Surgical approaches
In some cases, surgery may be recommended for severe motor fluctuations observed in PD depending on the symptoms present.
Therapeutic approaches
Therapeutic approaches also support people living with PD to manage symptoms of their disease:
- Occupational and physical therapies that are focused on balance and stretching exercises may help to maintain physical functioning throughout the progression of the disease.
- Speech therapy has also been found to help with the challenges of verbal communication – such as slurred speech – that can be associated with PD.
What about “Parkinson’s Plus” or atypical parkinsonisms?
According to the University of Cambridge Centre for Parkinson-Plus, "Parkinson-Plus syndromes...is a group of neurodegenerative diseases featuring the classical motor features of Parkinson's disease (tremor, rigidity, akinesia/bradykinesia, and postural instability) with additional features that distinguish them from...idiopathic Parkinson's disease (PD)."
In other words, as Alberta Health puts it, "Parkinson-plus syndromes are a group of neurological conditions that are similar to Parkinson's disease but have unique characteristics."
Parkinson-plus syndromes "can be hard to diagnose because the symptoms mimic other conditions," Alberta Health also notes.
Sometimes these syndromes are also called "atypical parkinsonisms."
The most common types of Parkinson-plus syndromes are
- dementia with Lewy bodies
- progressive supranuclear palsy
- multiple system atrophy
- cortical-basal degeneration
More information about dementia with Lewy bodies is available on our website, as is information about progressive supranuclear palsy and corticobasal degeneration.
For more information about multiple system atrophy, visit the Parkinson Canada website.
If you are concerned you may have a a Parkinson-Plus syndrome, make sure to speak to your doctor and also seek support from Parkinson Canada and your local Alzheimer Society.
More resources and downloads
Parkinson Canada. Parkinson Canada is the country's leading nonprofit organization looking to make a profound difference in the well-being of Canadians living with Parkinson’s disease.
For more information, read our print-friendly, downloadable brochure on Parkinson's disease.
This webpage was last updated on July 21, 2023. The related PDF download was last updated September 2021. If you have any concerns or feedback about the information on this webpage or download, please email publications@alzheimer.ca.
